Daclatasvir
BMS-790052,
EBP 883; BMS 790052
cas no 1009119-64-5
THERAPEUTIC CLAIM Treatment of hepatitis C
CHEMICAL NAMES
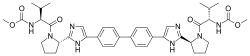
1. Carbamic acid, N,N'-[[1,1'-biphenyl]-4,4'-diylbis[1H-imidazole-5,2-diyl-(2S)-2,1-
pyrrolidinediyl[(1S)-1-(1-methylethyl)-2-oxo-2,1-ethanediyl]]]bis-, C,C'-dimethyl ester
2. dimethyl N,N'-(biphenyl-4,4'-diylbis{1H-imidazole-5,2-diyl-[(2S)-pyrrolidine-2,1-
diyl][(1S)-1-(1-methylethyl)-2-oxoethane-2,1-diyl]})dicarbamate
MOLECULAR FORMULA C40H50N8O6
MOLECULAR WEIGHT 738.9
SPONSOR Bristol-Myers Squibb
CODE DESIGNATION BMS-790052
CAS REGISTRY NUMBER 1009119-64-5
nmr
Daclatasvir dihydrochloride
THERAPEUTIC CLAIM Treatment of hepatitis C
CHEMICAL NAMES
1. Carbamic acid, N,N'-[[1,1'-biphenyl]-4,4'-diylbis[1H-imidazole-5,2-diyl-(2S)-2,1-
pyrrolidinediyl[(1S)-1-(1-methylethyl)-2-oxo-2,1-ethanediyl]]]bis-, C,C'-dimethyl ester,
hydrochloride (1:2)
2. dimethyl N,N'-(biphenyl-4,4'-diylbis{1H-imidazole-5,2-diyl-[(2S)-pyrrolidine-2,1-
diyl][(1S)-1-(1-methylethyl)-2-oxoethane-2,1-diyl]})dicarbamate dihydrochloride
MOLECULAR FORMULA C40H50N8O6 . 2 HCl
MOLECULAR WEIGHT 811.8
SPONSOR Bristol-Myers Squibb
CODE DESIGNATION BMS-790052-05
CAS REGISTRY NUMBER 1009119-65-6
Hepatitis C virus (HCV) is a major global health problem, with an estimated 150-200 million people infected worldwide, including at least 5 million in Europe (Pawlotsky, Trends Microbiol, 2004, 12: 96-102). According to the World Health Organization, 3 to 4 million new infections occur each year. The infection is often asymptomatic; however, the majority of HCV-infected individuals develop chronic infection (Hoof agle, Hepatology, 2002, 36: S21-S29; Lauer et al, N. Engl. J. Med., 2001, 345: 41-52; Seeff, Semin. Gastrointest., 1995, 6: 20-27). Chronic infection frequently results in serious liver disease, including fibrosis and steatosis (Chisari, Nature, 2005, 435: 930-932). About 20% of patients with chronic HCV infection develop liver cirrhosis, which progresses to hepatocellular carcinoma in 5% of the cases (Hoofnagle, Hepatology, 2002, 36: S21-S29; Blonski et al, Clin. Liver Dis., 2008, 12: 661-674; Jacobson et al, Clin. Gastroenterol. Hepatol, 2010, 8: 924-933; Castello et al., Clin. Immunol, 2010, 134: 237-250; McGivern et al., Oncogene, 2011, 30: 1969-1983).
Chronic HCV infection is the leading indication for liver transplantations (Seeff et al., Hepatology, 2002, 36: 1-2). Unfortunately, liver transplantation is not a cure for hepatitis C; viral recurrence being an invariable problem and the leading cause of graft loss (Brown, Nature, 2005, 436: 973-978; Watt et al, Am. J. Transplant, 2009, 9: 1707-1713). No vaccine protecting against HCV is yet available. Current therapies include administration of ribavirin and/or interferon-alpha (IFN-Cc), two non-specific anti-viral agents. Using a combination treatment of pegylated IFN-CC and ribavirin, persistent clearance is achieved in about 50% of patients with genotype 1 chronic hepatitis C. However, a large number of patients have contraindications to one of the components of the combination; cannot tolerate the treatment; do not respond to interferon therapy at all; or experience a relapse when administration is stopped. In addition to limited efficacy and substantial side effects such as neutropenia, haemo lytic anemia and severe depression, current antiviral therapies are also characterized by high cost. To improve efficacy of standard of care (SOC), a large number of direct acting antivirals (DAAs) targeting viral polyprotein processing and replication have been developed (Hofmann et al, Nat. Rev; Gastroenterol. Hepatol., 2011, 8: 257-264). These include small molecule compounds targeting HCV nonstructural proteins including the HCV protease, polymerase and NS5A protein. Although a marked improvement of antiviral response was observed when protease inhibitors were combined with SOC (Hofmann et al, Nat. Rev; Gastroenterol. Hepatol, 2011, 8: 257-264; Bacon et al, New Engl. J. Med., 2011, 364: 1207-1217; McHutchison et al, New Engl. J. Med., 2010, 362: 1292-1303; Poordad et al, New Engl. J. Med., 201 1, 364: 1195-1206; Hezode et al, New Engl. J. Med., 2009, 360: 1839-1850; Kwo et al, Lancet, 2010, 376: 705-716), toxicity of the individual compounds and rapid development of viral resistance in a substantial fraction of patients remain major challenges (Pawlotsky, Hepatology, 2011, 53: 1742-1751; Pereira et al, Nat. Rev. Gastroenterol. Hepatol., 2009, 6: 403-411; Sarrazin et al, Gastroenterol., 2010, 138: 447-462). New therapeutic approaches against HCV are therefore still needed. HCV entry into target cells is a promising target for antiviral preventive and therapeutic strategies since it is essential for initiation, spread, and maintenance of infection (Timpe et al, Gut, 2008, 57: 1728-1737; Zeisel et al, Hepatology, 2008, 48: 299-307). Indeed, HCV initiates infection by attaching to molecules or receptors on the surface of hepatocytes. Current evidence suggests that HCV entry is a multistep process involving several host factors including heparan sulfate (Barth et al, J. Biol. Chem., 2003, 278: 41003-41012), the tetraspanin CD81 (Pileri et al, Science, 1998, 282: 938-941), the scavenger receptor class B type I (SR-BI) (Zeisel et al, Hepatology, 2007, 46: 1722-1731; Bartosch et al, J. Exp. Med., 2003, 197: 633-642; Grove et al, J. Virol, 2007, 81 : 3162-3169; Kapadia et al, J. Virol, 2007, 81 : 374- 383; Scarselli et al, EMBO J., 2002, 21 : 5017-5025), Occludin (Ploss et al, Nature, 2009, 457: 882-886) and Claudin-1 (CLDN1), an integral membrane protein and a component of tight-junction strands (Evans et al, Nature, 2007, 446: 801-805). Furthermore, Niemann-Pick CI -like cholesterol absorption receptor has been identified as a new hepatitis C virus entry factor (Sainz et al, Nature Medicine, 2012, 18: 281-285).
Daclatasvir (USAN[1]) (formerly BMS-790052) is an experimental drug candidate for the treatment of hepatitis C. It is being developed by Bristol-Myers Squibb.
Daclatasvir's mechanism of action involves inhibition of the HCV nonstructural protein NS5A.[2][3] Recent research suggests that it targets two steps of the viral replication process, enabling rapid decline of HCV RNA.[4]
Daclatasvir has been tested in combination regimens with pegylated interferon and ribavirin,[5] as well as with other direct-acting antiviral agents including asunaprevir[6][7][8][9] and sofosbuvir.[10]

Daclatasvir (BMS-790052; EBP 883) is a first-in-class, highly-selective oral HCV NS5A inhibitor. NS5A is an essential component for hepatitis C virus (HCV) replication complex.Daclatasvir (BMS-790052; EBP 883)has broad genotype coverage and exhibits picomolar in vitro potency against genotypes 1a (EC50 50pm) and 1b (EC50 9pm).Daclatasvir (BMS-790052; EBP 883) produces a robust decline in HCV RNA (-3.6 logs after 48 hours from a single 100 mg) dosefollowing a single dose in patients chronically infected with HCV genotype 1.
It may be many years before the symptoms of hepatitis C infection appear. However, once they do, the consequences are significant: patients may have developed fibrosis, cirrhosis or even liver cancer, with the end result being liver failure. Even if diagnosed early, there’s no guarantee of a cure. Only around half of patients respond to the standard therapy of an interferon plus the antiviral drug ribavirin, and while two add-on antiviral therapies were approved in 2011, the treatment period is long with no guarantee of a cure, and for non-responders treatment options remain limited.
A new drug with a different mechanism is being developed by Bristol-Myers Squibb, in conjunction with Pharmasset. Daclatasvir targets non-structural protein 5A, which is an important component of the viral replication process, although its precise role in this remains unclear. The drug is active in single oral doses, and may have potential as part of a treatment regimen that avoids the use of interferon, and in patients who do not respond to standard therapy.
In an open label Phase IIa study, 10 patients with chronic hepatitis C genotype 1b infection who did not respond to standard therapy were given daclatasvir in once daily 60mg doses, plus another experimental drug, BMS-790052, which is an NSP 3 protease inhibitor, in initial twice-daily 600mg doses, later reduced to 200mg twice a day.2 Nine patients completed 24 weeks of treatment, with the 10th discontinuing after 10 weeks. In those who completed the course, HCV RNA was undetectable at week 8, and remained so until the end of the trial, with all achieving a sustained virologic response. It was also undetectable post-treatment in the patient who discontinued.
Daclatasvir has also been investigated as monotherapy in a double blind, placebo-controlled, sequential panel, multiple ascending dose study.3 Thirty patients with chronic geno-type 1 hepatitis C infection were randomised to receive a 14 day course of the drug, in once daily doses of 1, 10, 30, 60 or 100mg, 30mg twice a day, or placebo. There was no evidence of antiviral activity in the placebo group, but the mean maximum decline of 2.8 to 4.1 log IU/ml. Most experienced viral rebound on or before day 7 of treatment, which was associated with viral variants that had previously been implicated in resistance development. It was well tolerated in all dose groups.
M. Gao et al. Nature 2010, 465, 96

22/11/2013
European Medicines Agency advises on compassionate use of daclatasvir
Opinion concerns use in combination with sofosbuvir in patients with chronic hepatitis C in urgent need of therapy to prevent progression of liver disease
The European Medicines Agency’s Committee for Medicinal Products for Human Use(CHMP) has given an opinion on the use of daclatasvir in combination with sofosbuvir in the treatment of chronic (long-term) hepatitis C virus (HCV) infection, in a compassionate-use programme.
Compassionate-use programmes are set up at the level of individual Member States. They are intended to give patients with a life-threatening, long-lasting or seriously disabling disease with no available treatment options access to treatments that are still under development and that have not yet received amarketing authorisation. In this specific case, Sweden has requested an opinion from the CHMP on the conditions under which early access through compassionate use could be given to daclatasvir, for the use in combination with sofosbuvir, with or without ribavirin, for a specific patient population.
The recommended compassionate use is intended for adult patients at a high risk of their liver being no longer able to function normally (decompensation) or death within 12 months if left untreated, and who have a genotype 1 infection. Further, it is recognised that the potential benefit of such combination therapy may extend to patients infected with other HCV genotypes.
Daclatasvir and sofosbuvir are both first-in-class anti-viral medicines against HCV. These medicines have been studied in combination, with or without ribavirin, in aclinical trial which included treatment-naive (previously untreated) HCV genotype-1, -2 and -3 infected patients, as well as patients with genotype 1 infection who have previously failed telaprevir or boceprevir treatment. Results from the trial indicate high efficacy, also in those who have failed treatment with these protease inhibitors. Many such patients have very advanced liver disease and are in urgent need of effective therapy in order to cease the progression of liver injury.
This is the second opinion provided by the CHMP on compassionate use of medicines in development for the treatment of hepatitis C. Overall, it isthe fourth time compassionate use has been assessed by the CHMP.
The aim of the CHMP assessment and opinion on a compassionate-use programme for new medicinal products is to ensure a common approach, whenever possible, regarding the criteria and conditions of use under Member States' legislation. The opinion provides recommendations to the EU Member States that are considering setting up such a programme, and its implementation is not mandatory. In addition to describing which patients may benefit from the medicine, it explains how to use it and gives information on safety.
The assessment report and conditions of use of daclatasvir in combination with sofosbuvir with or without ribavirin in this setting will be published shortly on the Agency's website.
Notes
- The first compassionate-use opinion for a hepatitis C treatment was adopted by the CHMP in October 2013.
- Sofosbuvir, which is part of this compassionate-use opinion, received a positive opinion from the CHMP recommending granting of a marketing authorisation at its November 2013 meeting.
- Daclatasvir is developed by Bristol-Myers Squibb and sofosbuvir is developed by Gilead.
References
- ^ Statement on a Nonproprietary Name Adopted by the USAN Council
- ^ Gao, Min; Nettles, Richard E.; Belema, Makonen; Snyder, Lawrence B.; Nguyen, Van N.; Fridell, Robert A.; Serrano-Wu, Michael H.; Langley, David R.; Sun, Jin-Hua; O'Boyle, Donald R., II; Lemm, Julie A.; Wang, Chunfu; Knipe, Jay O.; Chien, Caly; Colonno, Richard J.; Grasela, Dennis M.; Meanwell, Nicholas A.; Hamann, Lawrence G. (2010). "Chemical genetics strategy identifies an HCV NS5A inhibitor with a potent clinical effect". Nature 465(7294): 96–100. doi:10.1038/nature08960. PMID 20410884.
- ^ Bell, Thomas W. (2010). "Drugs for hepatitis C: unlocking a new mechanism of action". ChemMedChem 5 (10): 1663–1665.doi:10.1002/cmdc.201000334. PMID 20821796.
- ^ Modeling shows that the NS5A inhibitor daclatasvir has two modes of action and yields a shorter estimate of the hepatitis C virus half-life. Guedj, J et al. Proceedings of the National Academy of Sciences. February 19, 2013.
- ^ AASLD: Daclatasvir with Pegylated Interferon/Ribavirin Produces High Rates of HCV Suppression. Highleyman, L. HIVandHepatitis.com. 6 December 2011.
- ^ Preliminary Study of Two Antiviral Agents for Hepatitis C Genotype 1. Lok, A et al. New England Journal of Medicine. 366(3):216-224. January 19, 2012.
- ^ "Bristol-Myers' Daclatasvir, Asunaprevir Cured 77%: Study". Bloomberg. Apr 19, 2012.
- ^ AASLD: Daclatasvir plus Asunaprevir Rapidly Suppresses HCV in Prior Null Responders. Highleyman, L. HIVandHepatitis.com. 8 November 2011.
- ^ High rate of response to BMS HCV drugs in harder-to-treat patients – but interferon-free prospects differ by sub-genotype. Alcorn, K. Aidsmap.com. 12 November 2012.
- ^ AASLD 2012: Sofosbuvir + Daclatasvir Dual Regimen Cures Most Patients with HCV Genotypes 1, 2, or 3. Highleyman, L. HIVandHepatitis.com. 15 November 2012.
https://www.google.co.in/patents/US20090041716?pg=PA1&dq=us+2009041716&hl=en&sa=X&ei=3ki4Uo-jEsTirAfzwoHQBQ&ved=0CD4Q6AEwAQ EXAMPLES A 1 L, 3-neck round bottom flask, fitted with a nitrogen line, overhead stirrer and thermocouple, was charged with 20 g (83.9 mmol, 1 equiv) 1,1′-(biphenyl-4,4′-diyl)diethanone, 200 mL CH2Cl2 and 8.7 mL (27.1 g, 169.3 mmol, 2.02 quiv) bromine. The mixture was allowed to stir under nitrogen for about 20 hours under ambient conditions. The resulting slurry was charged with 200 mL CH2Cl2 and concentrated down to about 150 mL via vacuum distillation. The slurry was then solvent exchanged into THF to a target volume of 200 mL via vacuum distillation. The slurry was cooled to 20-25° C. over 1 hour and allowed to stir at 20-25° C. for an additional hour. The off-white crystalline solids were filtered and washed with 150 mL CH2Cl2. The product was dried under vacuum at 60° C. to yield 27.4 g (69.2 mmol, 82%) of the desired product: 1H NMR (400 MHz, CDCl3) δ 7.95-7.85 (m, 4H), 7.60-7.50 (m, 4H), 4.26 (s, 4H); 13C NMR (100 MHz, CDCl3) 6 191.0, 145.1, 133.8, 129.9, 127.9, 30.8; IR (KBr, cm−1) 3007, 2950, 1691, 1599, 1199; Anal calcd for C16H12Br2O2: C, 48.52; H, 3.05; Br, 40.34. Found: C, 48.53; H, 3.03; Br, 40.53 HRMS calcd for C16H13Br2O2 (M+H; DCI+): 394.9282. Found: 394.9292. mp 224-226° C.A 500 mL jacketed flask, fitted with a nitrogen line, thermocouple and overhead stirrer, was charged with 20 g (50.5 mmol, 1 equiv) of Compound 2, 22.8 g (105.9 moles, 2.10 equiv) 1-(tert-butoxycarbonyl)-L-proline and 200 mL acetonitrile. The slurry was cooled to 20° C. followed by the addition of 18.2 mL (13.5 g, 104.4 mmol, 2.07 equiv) DIPEA. The slurry was warmed to 25° C. and allowed to stir for 3 hours. The resulting clear, organic solution was washed with 3×100 mL 13 wt % aqueous NaCl. The rich acetonitrile solution was solvent exchanged into toluene (target volume=215 mL) by vacuum distillation until there was less than 0.5 vol % acetonitrile.The toluene solution of Compound 3 was charged with 78 g (1.011 moles, 20 equiv) ammonium acetate and heated to 95-100° C. The mixture was allowed to stir at 95-100° C. for 15 hours. After reaction completion, the mixture was cooled to 70-80° C. and charged with 7 mL acetic acid, 40 mL n-butanol, and 80 mL of 5 vol % aqueous acetic acid. The resulting biphasic solution was split while maintaining a temperature >50° C. The rich organic phase was charged with 80 mL of 5 vol % aqueous acetic acid, 30 mL acetic acid and 20 mL n-butanol while maintaining a temperature >50° C. The resulting biphasic solution was split while maintaining a temperature >50° C. and the rich organic phase was washed with an additional 80 mL of 5 vol % aqueous acetic acid. The rich organic phase was then solvent exchanged into toluene to a target volume of 215 mL by vacuum distillation. While maintaining a temperature >60° C., 64 mL methanol was charged. The resulting slurry was heated to 70-75° C. and aged for 1 hour. The slurry was cooled to 20-25° C. over 1 hour and aged at that temperature for an additional hour. The slurry was filtered and the cake was washed with 200 mL 10:3 toluene:methanol. The product was dried under vacuum at 70° C., resulting in 19.8 g (31.7 mmol, 63%) of the desired product: 1H NMR (400 MHz, DMSO-d6) δ 13.00-11.00 (s, 2H), 7.90-7.75 (m, 4H), 7.75-7.60 (m, 4H), 7.60-7.30 (s, 2H), 4.92-4.72 (m, 2H), 3.65-3.49 (m, 2H), 3.49-3.28 (m, 2H), 2.39-2.1 (m, 2H), 2.10-1.87 (m, 6H), 1.60-1.33 (s, 8H), 1.33-1.07 (s, 10H); 13C NMR (100 MHz, DMSO-d6) δ 154.1, 153.8, 137.5, 126.6, 125.0, 78.9, 78.5, 55.6, 55.0, 47.0, 46.7, 33.7, 32.2, 28.5, 28.2, 24.2, 23.5; IR (KBr, cm−1) 2975, 2876, 1663, 1407, 1156, 1125; HRMS calcd for C36H45N6O4 (M+H; ESI+): 625.3502. Found: 625.3502. mp 190-195° C. (decomposed).To a 250 mL reactor equipped with a nitrogen line and overhead stirrer, 25.0 g of Compound 4 (40.01 mmol, 1 equiv) was charged followed by 250 mL methanol and 32.85 mL (400.1 mmol, 10 equiv) 6M aqueous HCl. The temperature was increased to 50° C. and agitated at 50° C. for 5 hours. The resulting slurry was cooled to 20-25° C. and held with agitation for about 18 hours. Filtration of the slurry afforded a solid which was washed successively with 100 mL 90% methanol/water (V/V) and 2×100 mL of methanol. The wet cake was dried in a vacuum oven at 50° C. overnight to give 18.12 g (31.8 mmol, 79.4%) of the desired product.Recrystallization of Compound 5 To a 250 mL reactor equipped with a nitrogen line and an overhead stirrer, 17.8 g of Compound 5 from above was charged followed by 72 mL methanol. The resulting slurry was agitated at 50° C. for 4 hours, cooled to 20-25° C. and held with agitation at 20-25° C. for 1 hour. Filtration of the slurry afforded a crystalline solid which was washed with 60 mL methanol. The resulting wet cake was dried in a vacuum oven at 50° C. for 4 days to yield 14.7 g (25.7 mmol, 82.6%) of the purified product: 1H NMR (400 MHz, DMSO-d6) δ 10.5-10.25 (br, 2H), 10.1-9.75 (br, 2H), 8.19 (s, 2H), 7.05 (d, J=8.4, 4H), 7.92 (d, J=8.5, 4H), 5.06 (m, 2H), 3.5-3.35 (m, 4H), 2.6-2.3 (m, 4H), 2.25-2.15 (m, 2H), 2.18-1.96 (m, 2H); 13C NMR (100 MHz, DMSO-d6) δ 156.6, 142.5, 139.3, 128.1, 127.5, 126.1, 116.9, 53.2, 45.8, 29.8, 24.3; IR (KBr, cm−1) 3429, 2627, 1636, 1567, 1493, 1428, 1028. Anal calcd for C26H32N6Cl4: C, 54.75; H, 5.65; Cl, 24.86; Adjusted for 1.9% water: C, 53.71; H, 5.76; N, 14.46; Cl, 24.39. Found: C, 53.74; H, 5.72; N, 14.50; Cl, 24.49; KF=1.9. mp 240° C. (decomposed).A 1 L jacketed flask equipped with a nitrogen line and an overhead stirrer was sequentially charged with 100 mL acetonitrile, 13.69 g (89.4 mmol, 2.5 equiv) hydroxybenzotriazole hydrate, 15.07 g (86 mmol, 2.4 equiv) N-(methoxycarbonyl)-L-valine, 16.46 g (85.9 mmol, 2.4 equiv) 1-(3-dimethyaminopropyl)-3-ethylcarbodiimide hydrochloride and an additional 100 mL acetonitrile. The resulting solution was agitated at 20° C. for 1 hour and charged with 20.4 g (35.8 mmol, 1 equiv) of purified Compound 5. The slurry was cooled to about 0° C. and 18.47 g (142.9 mmol, 4 equiv) diisopropylethylamine was added over 30 minutes while maintaining a temperature below 10° C. The solution was slowly heated to 15° C. over 3 hours and held at 15° C. for 12 hours. The resulting solution was charged with 120 mL 13 wt % aqueous NaCl and heated to 50° C. for 1 hour. After cooling to 20° C., 100 mL of isopropyl acetate was added. The biphasic solution was filtered through a 0.45 μm filter and the mixture split. The rich organic phase was washed with 2×240 mL of a 0.5 N NaOH solution containing 13 wt % NaCl followed by 120 mL 13 wt % aqueous NaCl. The mixture was then solvent exchanged into isopropyl acetate by vacuum distillation with a target volume of 400 mL. The resulting hazy solution was cooled to 20° C. and filtered through a 0.45 μm filter. The clear solution was then solvent exchanged into ethanol by vacuum distillation with a target volume of 140 mL. While maintaining a temperature of 50° C., 66.4 mL (82.3 mmol, 2.3 equiv) of 1.24M HCl in ethanol was added. The mixture was then charged with 33 mg (0.04 mmol, 0.001 equiv) of seed crystals of Compound (I) (see preparation below) and the resulting slurry was stirred at 50° C. for 3 hours. The mixture was cooled to 20° C. over 1 hour and aged at that temperature for an additional 22 hours. The slurry was filtered and the wet cake was washed with 100 mL of 2:1 acetone:ethanol. The solids were dried in a vacuum oven at 70° C. to give 22.15 g (27.3 mmol, 76.3%) of the desired product.A solution of Compound (I) was prepared by dissolving 3.17 g of Compound (I) from above in 22 mL methanol. The solution was passed through a 47 mm Cuno Zeta Carbon® 53SP filter at ˜5 psig at a flow rate of ˜58 mL/min. The carbon filter was rinsed with 32 mL of methanol. The solution was concentrated down to 16 mL by vacuum distillation. While maintaining a temperature of 40-50° C., 15.9 mL acetone and 5 mg of seed crystals of Compound (I) (see procedure below) were added. The resulting slurry was then charged with 32 mL acetone over 30 minutes. The slurry was held at 50° C. for 2 hours, cooled to 20° C. over about 1 hour and held at 20° C. for about 20 hours. The solids were filtered, washed with 16 mL 2:1 acetone:methanol and dried in a vacuum oven at 60° C. to give 2.14 g (67.5%) of purified Compound (I): 1H NMR (400 MHz, DMSO-d6, 80° C.): 8.02 (d, J=8.34 Hz, 4 H), 7.97 (s, 2 H), 7.86 (d, J=8.34 Hz, 4 H), 6.75 (s, 2 H), 5.27 (t, J=6.44 Hz, 2 H), 4.17 (t, J=6.95 Hz, 2 H), 3.97-4.11 (m, 2 H), 3.74-3.90 (m, 2 H), 3.57 (s, 6 H), 2.32-2.46 (m, 2 H), 2.09-2.31 (m, 6 H), 1.91-2.07 (m, 2 H), 0.88 (d, J=6.57 Hz, 6 H), 0.79 (d, J=6.32 Hz, 6 H); 13C NMR (75 MHz, DMSO-d6): δ 170.9, 156.9, 149.3, 139.1, 131.7, 127.1, 126.5, 125.9, 115.0, 57.9, 52.8, 51.5, 47.2, 31.1, 28.9, 24.9, 19.6, 17.7; IR (neat, cm−1): 3385, 2971, 2873, 2669, 1731, 1650. Anal. Calcd for C40H52N8O6Cl2: C, 59.18; H, 6.45; N, 13.80; Cl, 8.73. Found C, 59.98; H, 6.80; N, 13.68; Cl, 8.77. mp 267° C. (decomposed).![Figure US20090041716A1-20090212-C00014]()
- https://www.google.co.in/patents/US20090041716?pg=PA1&dq=us+2009041716&hl=en&sa=X&ei=3ki4Uo-jEsTirAfzwoHQBQ&ved=0CD4Q6AEwAQ
- [0152]BMS-791325 preferably is
As used herein, BMS-791325 may also be
See also publications at http://wwwl.easl.eu/eas12011/program/Posters/Abstract680.htm; and http://clinicaltrials.gov/show/NCT00664625. For GS-5885, see publications at http://www.natap.org/2011/EASL/EASL_68.htm; http://wwwl.easl.eu/eas12011/program/Posters/Abstract1097.htm; and http://clinicaltrials.gov/ct2/show/NCT01353248.
Compound 1(
) or a pharmaceutically acceptable salt thereof. Compound 1 is also known as (2R,6S,13aS,14aR,16aS,Z)-N-(cyclopropylsulfonyl)-6-(5-methylpyrazine-2-carboxamido)-5,16-dioxo-2-(phenanthridin-6-yloxy)-1,2,3,5,6,7,8,9,10,11,13a,14,14a,15,16,16a-hexadecahydrocyclopropa[e]pyrrolo[1,2-a][1,4]diazacyclopentadecine-14a-carboxamide. Compound 1 is a potent HCV protease inhibitor. The synthesis and formulation of Compound 1 are described inU.S. Patent Application Publication No. 2010/0144608 , U.S. Provisional Application Serial No. 61/339,964 filed on March 10, 2010 U.S. Patent Application Publication No. 2011/0312973 filed on March 8, 2011
) or a pharmaceutically acceptable salt thereof. Compound 1 is also known as (2R,6S,13aS,14aR,16aS,Z)-N-(cyclopropylsulfonyl)-6-(5-methylpyrazine-2-carboxamido)-5,16-dioxo-2-(phenanthridin-6-yloxy)-1,2,3,5,6,7,8,9,10,11,13a,14,14a,15,16,16a-hexadecahydrocyclopropa[e]pyrrolo[1,2-a][1,4]diazacyclopentadecine-14a-carboxamide. Compound 1 is a potent HCV protease inhibitor. The synthesis and formulation of Compound 1 are described in




































